Image Credit: Getty Image
Bibasilar atelectasis is a medical condition that often flies under the radar, yet its impact on respiratory health cannot be overstated. Manifesting as the partial collapse of the lung bases, it raises questions such as “is it normal to have bibasilar atelectasis?” or “is bibasilar atelectasis serious?” Given the prevalence of minimal bibasilar atelectasis on CT scan findings, especially in settings like post-operative recovery or in the context of diseases such as COVID-19, understanding this condition becomes pivotal. Its identification, though often incidental, underscores the need for awareness and clarity about its implications and the potential for it to progress from a mild to a more concerning level.
The subsequent sections of this article will delve deeper into defining what bibasilar atelectasis is, drawing attention to its causes, symptoms, and the populations most at risk. Addressing concerns regarding how mild bibasilar atelectasis on CT scan findings should be interpreted, we will explore the diagnostic approaches that healthcare providers take, including the significance of the bibasilar atelectasis ICD 10 classification. Finally, we will review the therapy and management options available to those diagnosed, highlighting how treatment can vary depending on the severity and underlying causes of the atelectasis. By offering a comprehensive overview, this article aims to demystify bibasilar atelectasis and provide valuable insights into its diagnosis and treatment.
What is Bibasilar Atelectasis?
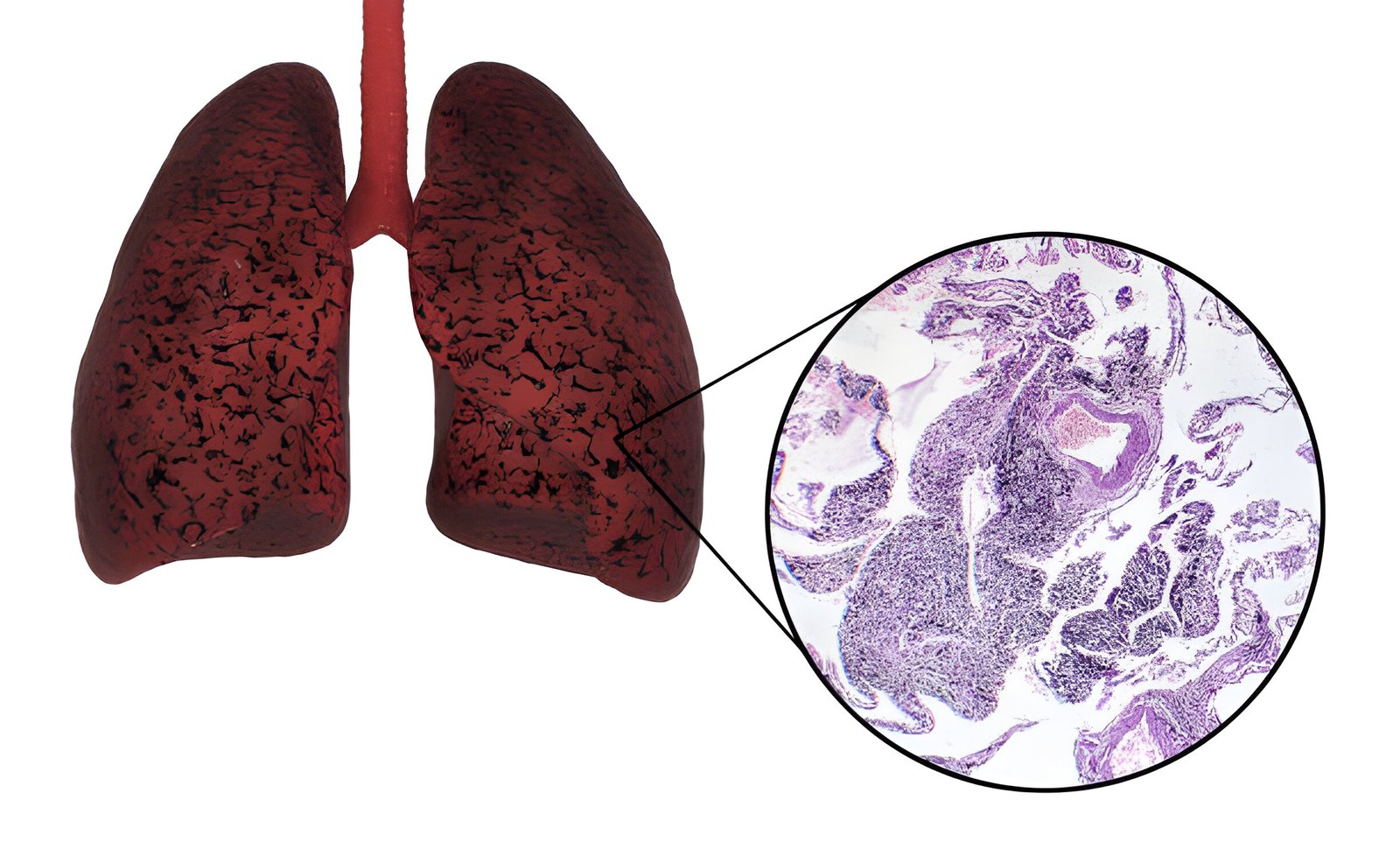
Bibasilar atelectasis refers to the partial collapse of the lower sections of both lungs. This condition is significant because it affects the alveoli, the tiny air sacs in the lungs responsible for the exchange of oxygen and carbon dioxide during breathing. When these air sacs deflate, it can lead to reduced oxygen levels in the blood and difficulty breathing.
Overview of the Condition
Bibasilar atelectasis can manifest in various forms, ranging from mild to severe. In its more severe form, it can resemble conditions like pneumothorax, where a complete lung collapse occurs. Symptoms typically associated with bibasilar atelectasis include difficulty breathing, coughing up mucus, and in some cases, wheezing. The impact on an individual’s respiratory function can vary, depending on the extent of the collapse and the underlying cause.
Causes of Bibasilar Atelectasis
The causes of bibasilar atelectasis can be categorized into obstructive and non-obstructive types. Obstructive causes occur when there is a physical blockage in the airways. Common obstructive causes include:
- Mucus Plug: Accumulation of mucus in the airways, often following surgery, can block the air passage.
- Foreign Objects: Inhaled objects can obstruct the airways, more commonly seen in children.
- Tumors: Abnormal growths can narrow or block airways, restricting airflow.
- Blood Clots: Occurring typically after significant pulmonary bleeding, clots can obstruct the airways.
Non-obstructive causes, on the other hand, result from external pressure on the lungs that prevents normal expansion during inhalation. These include:
- General Anesthesia: Changes in regular breathing patterns during surgery can lead to alveolar collapse.
- Pleural Effusion: Fluid accumulation in the lung cavity exerts pressure on the lungs, hindering their ability to expand fully.
- Chest Trauma: Injuries to the chest can compress the lungs and restrict their movement.
- Pneumothorax: Air leakage into the space between the lungs and chest wall can collapse the lung.
- Lung Infections and Scar Tissue: Both can cause inflammation or fibrosis, which physically restricts lung expansion.
Understanding these causes is crucial for diagnosing and managing bibasilar atelectasis effectively, as treatments are typically tailored to address the specific underlying cause.
Symptoms and Risk Factors
Primary Symptoms
Bibasilar atelectasis manifests through a variety of symptoms, which can range from mild to severe depending on the extent of the lung collapse. Individuals may experience difficulty breathing, often described as a shortness of breath or an inability to take a full, satisfying breath. This is medically referred to as dyspnea. Additional respiratory symptoms include rapid or shallow breathing, wheezing, and a persistent cough that produces a significant amount of mucus. In some cases, individuals might hear crackling sounds while breathing or notice an absence of breath sounds in severe instances.
Symptoms tend to develop suddenly and can worsen as the condition progresses, leading to plummeting oxygen levels in the blood. It’s crucial to recognize these symptoms early, as they are indicative of the reduced airway capacity and the body’s struggle to maintain adequate oxygenation.
High-Risk Groups
The likelihood of developing bibasilar atelectasis increases with certain risk factors that can exacerbate the condition. Age is a significant factor; older adults are more susceptible due to the natural decline in lung capacity and resilience. Additionally, both obesity and pregnancy are known to exert pressure on the diaphragm and lungs, which can compromise the respiratory system and lead to atelectasis.
Smoking is another critical risk factor that not only increases the risk of developing lung diseases but also contributes to the occurrence of atelectasis by impairing respiratory function and mucus clearance. Prolonged bed confinement or immobility and extended durations under general anesthesia during surgery are also notable risk factors. These situations can lead to a decrease in respiratory movements and a buildup of mucus, further obstructing the airways and leading to lung collapse.
Understanding these risk factors is essential for both individuals and healthcare providers to prevent the onset of bibasilar atelectasis and to manage the condition effectively should it occur.
Also visit: Amoxicillin Side Effects in Women: Symptoms and Prevention
Approaches to Diagnosis
Initial Medical Examination
When a healthcare provider suspects bibasilar atelectasis, a comprehensive physical examination is typically the first step. During this examination, the provider listens for diminished breathing sounds, particularly in the lower lung areas, which may indicate a collapse. This initial assessment often includes a review of the patient’s medical history and recent treatments to identify any contributing factors.
A chest X-ray is commonly employed to visualize abnormalities in the lungs and chest that are indicative of atelectasis. This imaging technique can reveal characteristic signs such as platelike, horizontal lines or displacement of interlobar fissures, which are suggestive of atelectatic lung tissue. Despite its utility, a chest X-ray may not always show atelectasis until it is significant, prompting the need for more detailed imaging.
Advanced Diagnostic Tools
For a more precise diagnosis, several advanced diagnostic tools are utilized:
- Computed Tomography (CT) Scan: A CT scan offers a more detailed view than a standard X-ray and is better at identifying the type and cause of atelectasis. It can reveal dependent lung densities and loss of volume in the affected side, providing crucial details that guide further management.
- Chest Ultrasound: This non-invasive test uses sound waves to create detailed images of the chest’s internal structures. It is particularly useful for identifying conditions like pneumothorax and pleural effusion, which can lead to atelectasis.
- Bronchoscopy: This procedure involves inserting a flexible, lighted tube through the throat to directly view the airways and lungs. It is essential for identifying obstructions such as mucus plugs, tumors, or foreign bodies that could be causing the atelectasis. Bronchoscopy can also be therapeutic, allowing for the removal of blockages.
- Oximetry: A simple and quick test, oximetry measures blood oxygen levels using a small device placed on the finger. It helps assess the severity of atelectasis by determining how much the lung collapse has affected oxygenation.
- Positron Emission Tomography (PET): Although not routinely used for diagnosing atelectasis, PET scans can detect changes in cellular metabolism suggestive of more serious conditions like lung cancer, which may present similarly.
By utilizing these diagnostic tools, healthcare providers can confirm the presence of bibasilar atelectasis, understand its severity, and identify any underlying causes, which are critical for planning effective treatment strategies.
Therapy and Management Options
Breathing Techniques
Effective management of bibasilar atelectasis often includes the implementation of targeted breathing exercises designed to improve lung function and enhance oxygen intake. Pulmonary rehabilitation specialists emphasize the importance of exercises like pursed lip breathing and belly breathing for individuals with chronic lung conditions. These techniques facilitate the expulsion of stale air and promote the intake of fresh air, thereby making the lungs more efficient.
- Pursed Lip Breathing: This technique involves breathing in through the nose and exhaling at least twice as long through pursed lips. It is particularly beneficial in slowing down the breathing rate, which allows for better air exchange in the lungs.
- Belly Breathing: Also known as diaphragmatic breathing, this method focuses on the diaphragm’s role in breathing. Individuals are encouraged to pay attention to the belly rising and falling with each breath, which helps in maximizing air distribution in the lungs. This can be practiced by placing a light object like a tissue box on the stomach to visualize the correct movement.
Both exercises should ideally be practiced daily for about 5 to 10 minutes to achieve the best results. Starting these exercises when breathing is not severely compromised allows individuals to utilize them effectively during episodes of shortness of breath.
Medical Treatments
The medical approach to treating bibasilar atelectasis depends on the underlying cause. If the atelectasis is due to an obstruction, treatments may involve removing the blockage through various methods:
- Medications: These include bronchodilators and mucolytic agents that help open airways and thin mucus respectively, facilitating easier breathing.
- Suctioning: Excess mucus may be removed through suctioning, allowing for deeper breaths and clearer airways.
- Surgery: In cases where tumors or other physical obstructions are present, surgical interventions may be necessary.
Additional supportive treatments may include the use of supplemental oxygen to enhance breathing or antibiotics to address any infections that might complicate the condition. Regular monitoring and follow-up are crucial, especially for individuals with risk factors or persistent symptoms. This ensures that any changes in the condition can be promptly addressed, and appropriate adjustments to the treatment plan can be made.
In cases where the atelectasis is not caused by a blockage, other techniques such as incentive spirometry may be recommended. This involves deep breathing exercises that encourage the lungs to expand and prevent fluid accumulation. Physical therapy can also be beneficial in promoting lung expansion and improving overall respiratory health.
Implementing these therapy and management options under the guidance of healthcare professionals ensures a comprehensive approach to treating bibasilar atelectasis, ultimately improving the patient’s respiratory function and quality of life.
Also visit: Aseptic Technique: Detailed Instructions and Best Practices
Conclusion
Through this article, we’ve taken a comprehensive journey to understand bibasilar atelectasis, from its symptoms and causes to the various treatment options available. Focusing on the significance of early diagnosis and tailored therapies, it becomes clear that understanding the nuances of this condition is integral to improving patient outcomes. Emphasizing the critical role of both non-invasive and advanced diagnostic tools, we see how significant it is to identify the underlying causes of atelectasis to ensure effective management. This exploration has not only shed light on the medical strategies deployed to combat bibasilar atelectasis but has also underscored the importance of self-management techniques such as targeted breathing exercises.
The dialog around bibasilar atelectasis serves as a reminder of the delicacy of our respiratory health and the importance of maintaining it through preventive measures and timely intervention. By recognizing the symptoms early and understanding the risk factors, individuals can seek the appropriate care and treatment necessary to mitigate complications. Moreover, this article champions the idea that both patients and healthcare providers play pivotal roles in navigating the challenges associated with bibasilar atelectasis. From fostering awareness to implementing comprehensive care strategies, the collective effort is crucial in enhancing the lives of those affected by this condition, offering a beacon of hope towards better respiratory health and overall well-being.
FAQs
Q: What are the treatment options for Bibasilar atelectasis?
A: Bibasilar atelectasis is typically diagnosed through a physical examination, imaging tests like X-rays or CT scans, and sometimes a bronchoscopy, which is a minimally invasive procedure. Treatments include performing breathing exercises, clearing the airways, and using medications that help dilate the airways and liquefy mucus.
Q: What are the most effective treatments for atelectasis?
A: Effective treatments for atelectasis include deep breathing exercises using devices like incentive spirometers, removing blockages in the lungs often through bronchoscopy, physical therapy to aid lung expansion, inhaling medications to dilate the airways, and managing any underlying conditions like tumors or chronic lung diseases.
Q: Which medication is considered best for treating atelectasis?
A: Albuterol, available under brand names like Proventil and Ventolin, is widely used to treat atelectasis. It is an inhaled beta-agonist that helps open up the airways, and it is usually prescribed on an as-needed basis, benefiting most patients even if they do not show a measurable increase in expiratory flow.
Q: How is atelectasis managed in patients?
A: Managing atelectasis involves suctioning mucus or performing a bronchoscopy to remove blockages in the airways. During a bronchoscopy, a flexible tube is inserted down the throat to clear the airways. If atelectasis is caused by a tumor, the treatment may involve surgical intervention to remove or reduce the size of the tumor during the bronchoscopy.


Leave a Reply